DONATE

What is C5-Rural
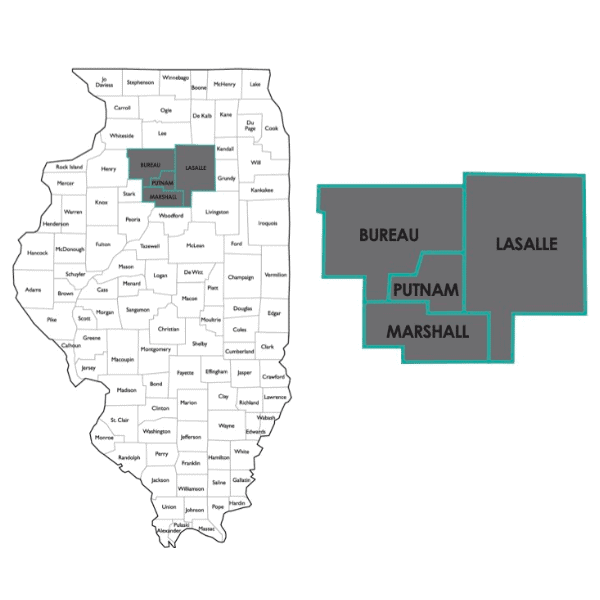
C5-Rural is a collaborative healthcare network with members from Lasalle, Bureau, Marshall and Putnam counties in the state of Illinois with the purpose of bringing together primary care providers, mental health providers, complementary care and community-based providers in order to develop integrative care strategies that bridge gaps in rural mental health and substance use prevention, treatment and recovery in new and innovative ways. C5-Rural will achieve efficiencies, coordinate and improve the quality of behavioral healthcare services, and expand access to services that treat social determinants of health. Collaborative mental health care is an evidence-based, research-driven paradigm that acknowledges the legitimacy of conventional as well as select complementary and community services, recommending specific treatment combinations supported by research findings. Using all available options we will expand the type of currently available behavioral healthcare for rural people, by providing person-centered care that focuses on the whole person, emphasizing wellness and lifestyle while addressing the range of complex biological, social-emotional, psychological, cultural, and spiritual/religious factors that are determinants of mental health.
The Need
Lasalle, Bureau, Marshall and Putnam counties exhibit abnormally high mental illness, suicide, and disability due to mental illness or substance use disorder, and these areas are federally-designated health professional shortage areas in primary care and mental health. Current models of mental health care and treatment options fall short of adequately addressing the need. “Mental health” and “wellness” have been prioritized on county-wide health assessments for more than a decade, and few sustainable solutions have come forth.
The first populations of focus are youth and young adults, ages 12-35 years. Our data show that approximately 40% of all suicide attempts in our region occur in this age range, and 84% of teen survey respondents report past or present struggles with depression, suicidal thoughts, or extreme/prolonged stress or anxiety with less than half receiving necessary help. As we approach these needs as a network, our data show that we must pay careful attention to using age- and culturally-relevant information sharing mechanisms, providing social support and mentoring, finding ways to overcome the inordinate stigma, and providing services regardless of one’s ability to pay. Moreover, to truly meet the need, our network is designing ways to help our youth prioritize their own health and wellness, empowering them to self-drive their own care rather than passively receiving care in a clinician’s office.
Our data shows that approximately 40% of all suicide attempts in our region occur in youth and young adults ages 12-35, and 84% of teen survey respondents report past or present struggles with depression, suicidal thoughts, or extreme/prolonged stress or anxiety with less than half receiving necessary help.
This effort was supported by a Rural Health Network Planning Program grant from the U.S. Department of Health and Human Services (HHS), Health Resources and Service Administration (HRSA), Federal office of Rural Health Policy (FORHP), Community-Based Division (CBD), Award No. P10RH33037; a 2020 Rural Communities Opioid Response Program (RCORP) Planning grant, Award No. G25RH40024 from HHS/HRSA FORHP; and is currently supported by a 2020 Drug-Free Communities grant from the White House Office of National Drug Control Policy (ONDCP) and Centers for Disease Control and Prevention, Award No. NH28CE003019. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, ONDCP, CDC, or the U.S. Government.

contact us today
ABOUT US
Arukah brings accessible & relational holistic complementary health and mental health care to rural communities
LANGUAGE ASSISTANCE
VISIT US
1916 North Main St., Suite 3
Princeton, Illinois 61356
Open Monday - Friday 8am - 6pm
(815) 872-2943
Transactions on this website are being processed securely by one of the most trusted names in the payments industry.

